
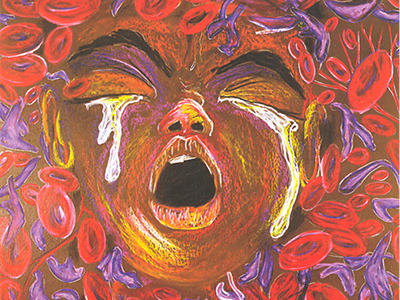
Duke CTSI announces the publication of a new case study, "Biopsychosocial Determinants of Pain in Sickle Cell Disease," a research study led by Dr. Mitchell Knisely of the Duke University School of Nursing.
This case study discusses not only the methods and results of the research, but explores the challenges the researchers faced and the strategies they employed to overcome those challenges. It also clearly demonstrates the benefits to patients and society of this translational science project.
Here is the Knisely Case Study using the Translational Science Benefits Model.

Principal Investigator: Mitchell Knisely
Additional Investigators: Nirmish Shah and Qing Yang
Year funded: June 2019- June 2020
Latest Updates: The CTSI Integrating Special Populations Award was able to support the initial recruitment of 48 participants. However, given the success of recruitment and ability to contain costs, Knisely was able to recruit a total of 73 participants for the CTSI study. Furthermore, Knisely was able to secure additional funding to continue sample collection. In total, biospecimens/DNA samples was collected from 94 individuals.
Scope: Sickle cell disease (SCD) is a rare disease that negatively affects people from underrepresented minorities. Pain is a common and debilitating symptom experienced across the lifespan by people with sickle cell disease, Few effective treatments exist, resulting in opioids being a first-line treatment for this population. Specific aims for this exploratory, cross-sectional study of individuals who are 15 years and older and have SCD are to: (1) test the feasibility of blood specimen collection over a 6-month time frame; and (2) determine three pain phenotypes (i.e., no pain, episodic severe pain, persistent severe pain) based upon participant responses to a validated SCD pain measure asking the occurrence of severe pain in the last six months. Blood specimens will be collected from individuals with sickle cell disease and health controls to generate inflammatory biomarker data. Refined processes for blood collection in an underrepresented sample are already enrolled in an existing research registry.
Publication Severe Persistent Pain and Inflammatory Biomarkers in Sickle Cell Disease: A Exploratory Study
Conferences: (Dates TBA)
Video Profile: Highlighting the impact of Mitch Knisely's pilot, pilot findings, challenges with implementing a SCD registry, and lessons learned when adding a biospecimen collection to a SCD registry.
Investigators: Sudha Raman and Charlene Wong
Year funded: April 2019-March 2020
Scope: The opioid epidemic includes children and adolescents, and there is a need to develop a local, evidence-based plan to address opioid exposures and harms among this vulnerable population. The objective of this pilot is to document the patterns of opioid prescriptions and opioid-related harms to children in North Carolina. The investigators seek to discover NC-specific patterns in a vulnerable population of low-income children, focusing on disparities by geographic region and the following age groups: infants (<2), early childhood (2-5), school age (6-11), and adolescents (12-18). This project will utilize Medicaid claims from 2013-2018 to study pediatric opioid exposure, sources of prescribed opioids, adn opioid-related harms, such as hospitalizations and emergency department visits.
Publications:
Conferences:

Contact XYZ for more information on accessing Medicaid claims data.